How can dynamic stretch benefit you?
Stretching is important because it increases flexibility, improves posture and balance and can prevent falls. Stretching should be done consistently and it’s best if you can make it a part of your daily routine.
WHY IS STRETCHING IMPORTANT?
Increasing range of motion
when you increase your flexibility it keeps you more mobile and makes performing yoru daily activities easier
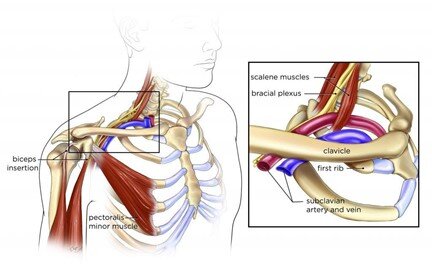
Helps to prevent aches and pains
flexibility throughout your muscles encourages optimal use- like maintaining proper posture at your computer/desk all day and can help to prevent come things like a sore neck and back
Decrease overuse injuries
as you use your muscles they get tighter and shorter, tight short muscles do not perform as well as flexible ones
people who perform repetitive tasks or movements, do a lot of lifting/pushing/pulling should really work on making time to stretch in order to prevent injuries
Improves overall performance
joints work best when they are flexible and muscles work best when they are long
tight muscles just don’t have the same explosive power as one with more length/flexibility